The Centre for Youth Bipolar Disorder is back with part 2 of our blog series on our exercise study for improving aerobic fitness in teens with bipolar disorder (see part 1 here). In this blog, we will share first-hand knowledge that we have gained from 11 teen participants, who completed the full intervention in Toronto, Ontario, and were invited back to participate in a consultation forum to share their experiences and provide feedback. The observations and feedback from 5 parents will also be shared. Participant names were removed to protect confidentiality.
Feedback from the teen participants
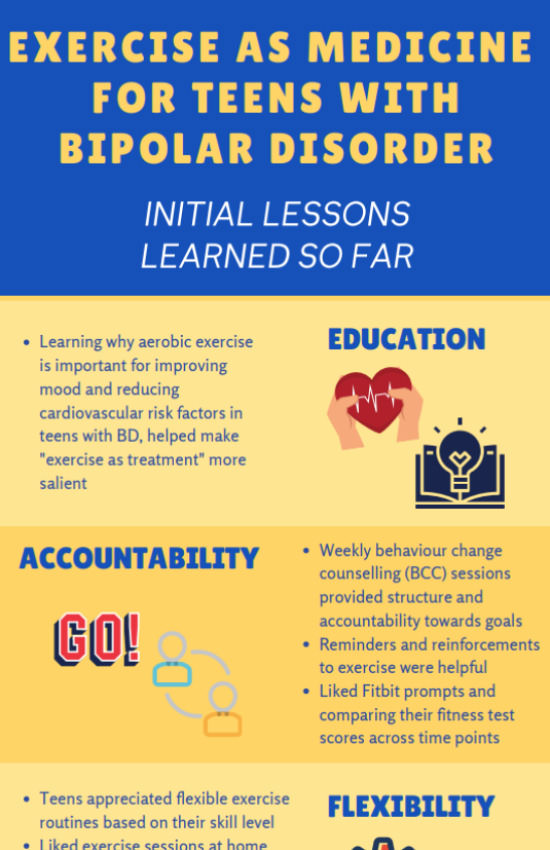
Education:
The first behaviour change counselling (BCC) session in the study provides psychoeducation on the links between bipolar disorder (BD), exercise, mood, and heart health. Several participants already knew that physical activity can boost mental health, although were surprised to learn how important heart health is for people living with BD. Learning these facts helped make the concept of “exercise as treatment” more salient and meaningful to them.
“I didn’t know how [activity and bipolar disorder] were intertwined until I was told those details…that allowed me to understand how important it is to take it as treatment, and not just as like, “oh it’s a chore, it’s exercise.” – Participant, age 17.
Accountability:
BCC sessions were delivered weekly for the first 12 weeks of the study, with the goal of improving aerobic fitness by targeting teens’ motivation and commitment to change and identifying personal fitness goals and barriers. Participants agreed that the first 12 weeks provided a great deal of structure and accountability for maintaining their exercise goals. Weekly check-ins (via phone or text) acted as reminders and reinforcement for keeping them on track (“I need to exercise at least twice before that call”). In fact, a general consensus among participants was that they appreciated the structure and accountability of the first 12 weeks, and missed having this during weeks 13-24, where they were ‘independent exercisers’ and only received 2 booster calls/texts. In addition, all participants received a Fitbit to track their steps and heart rate. Some found the Fitbit reminders helpful in keeping them moving, and they enjoyed seeing their progress in the app.
“I really liked when there were the phone calls, cause it was kind of like a reminder and kind of reinforcing …kind of like motivation and reminding me to go and exercise.” – Participant, age 17.
Flexibility:
 Several participants appreciated the flexible approach towards building exercise goals and being encouraged to choose cardiovascular activities that they enjoyed. Some participants said that the texting option for phone sessions made it easier to check in with their therapist and thought of it as “a transcript” of their conversation on their phone (“With texting it’s a lot more convenient, so I could get it done while I was studying at the library…”). Flexibility was bolstered by the study kinesiologist or ‘exercise expert’, who was available to exercise with teens as per their preference (e.g., at a gym, in-person at their home) and teach them exercises they could do independently. Participants learned and valued the concept that exercise could occur in short and regular intervals, which opposed their belief that it had to be in long intervals.
Several participants appreciated the flexible approach towards building exercise goals and being encouraged to choose cardiovascular activities that they enjoyed. Some participants said that the texting option for phone sessions made it easier to check in with their therapist and thought of it as “a transcript” of their conversation on their phone (“With texting it’s a lot more convenient, so I could get it done while I was studying at the library…”). Flexibility was bolstered by the study kinesiologist or ‘exercise expert’, who was available to exercise with teens as per their preference (e.g., at a gym, in-person at their home) and teach them exercises they could do independently. Participants learned and valued the concept that exercise could occur in short and regular intervals, which opposed their belief that it had to be in long intervals.
“I thought the exercise expert was great. Especially because she went above and beyond what I asked for, with the whole customized workout schedule.” – Participant, age 19.
Even though teens valued flexibility, especially with their busy schedules, some suggested that exercise coaching should have been mandatory, and in general felt the need for more structure and expectations. Once the active phase of treatment was over, following the 12 week mark, participants often felt lost about what to do with regards to exercise without the structure of in-person exercise sessions and phone sessions with their therapist.
“If there was like more of a push, like you need to be like with an instructor, or you need to at least move up 1 level …that would’ve pushed me more to work out with the exercise expert, instead of working out by myself or with friends.” – Participant, age 16.
Desire for Additional Detail and Reminders about Optional Modules:
Teen participants offered feedback that it would have been helpful to have more detailed descriptions of the optional modules available to them (e.g., exercise coaching and peer support). For example, they would have liked more clarification around the role of the exercise expert, as what was in fact available to participants was more diverse than their initial perceptions of an “exercise trainer”. Others reported that they lost track of what optional modules were available to them and how they worked, and suggested that providing more reminders and presenting the optional modules in a concise reference sheet could be helpful.
Feedback from the parents
Importance of “Exercise as Medicine” Concept:
Several parents commented on the importance of positioning exercise as a full-fledged component of treatment, rather than a casual recommendation.
“I thought it was really important that it was couched as part of their medical therapy, that it wasn’t just something we think was fun or cool or whatever…it’s part of the whole therapy. You see the therapist, you see your psychiatrist, you take your medication, and you exercise.” – Parent of participant, age 19.
Value of the Exercise Expert:
Parents shared that the study’s exercise expert helped to keep their teen accountable, consistent, and motivated to stick to their exercise goals. Another parent appreciated that the exercise expert used a personalized approach with their teen. By extension, the parents shared that they appreciated how the exercise intervention and exercise expert took the ‘responsibility’ of motivating their teen to exercise off their hands. One parent suggested that it would be helpful for the exercise expert to do regular check-ins with their teen, similar to the phone sessions delivered by the study therapist. One parent was struck by the detrimental effect of depression symptoms on her teen’s motivation, and went on convey that she thought it would make all the difference to have an assigned personal exercise expert as part of regular clinical treatment.
Mood and Motivation:
 Several parents reported that depression was the most difficult barrier to exercise, and that consistent exercise during an interval of depression was extraordinarily difficult to maintain. This often related to their teens not having motivation to follow through with their exercise plan. Another parent shared that they saw a positive and significant difference in their teen’s demeanor and energy levels after beginning the intervention, but that this change was difficult to maintain after the first 12 weeks.
Several parents reported that depression was the most difficult barrier to exercise, and that consistent exercise during an interval of depression was extraordinarily difficult to maintain. This often related to their teens not having motivation to follow through with their exercise plan. Another parent shared that they saw a positive and significant difference in their teen’s demeanor and energy levels after beginning the intervention, but that this change was difficult to maintain after the first 12 weeks.
Family Engagement:
Participants had the option of involving their family in their BCC or exercise sessions. One parent attended a BCC session in order to show support for their teen, and shared that they appreciated getting to see and interact with the study therapist. Another parent shared that while their teen didn’t include them in any of the modules, they would have been eager to participate as a way to show support and provide motivation. A general consensus with the parents was that they believed that their own exercise habits don’t influence their teen’s exercise behaviours, however one parent shared that their teen influenced them to re-start exercise with an app that they learned about from the exercise expert. As not all teens included their parents, some parents expressed a desire to receive feedback about what was happening in sessions in order to support their teen.
Stay tuned for part 3, where our patient collaborator will share her thoughts and perspective on the intervention and exercise for youth with BD.







Leave a Reply